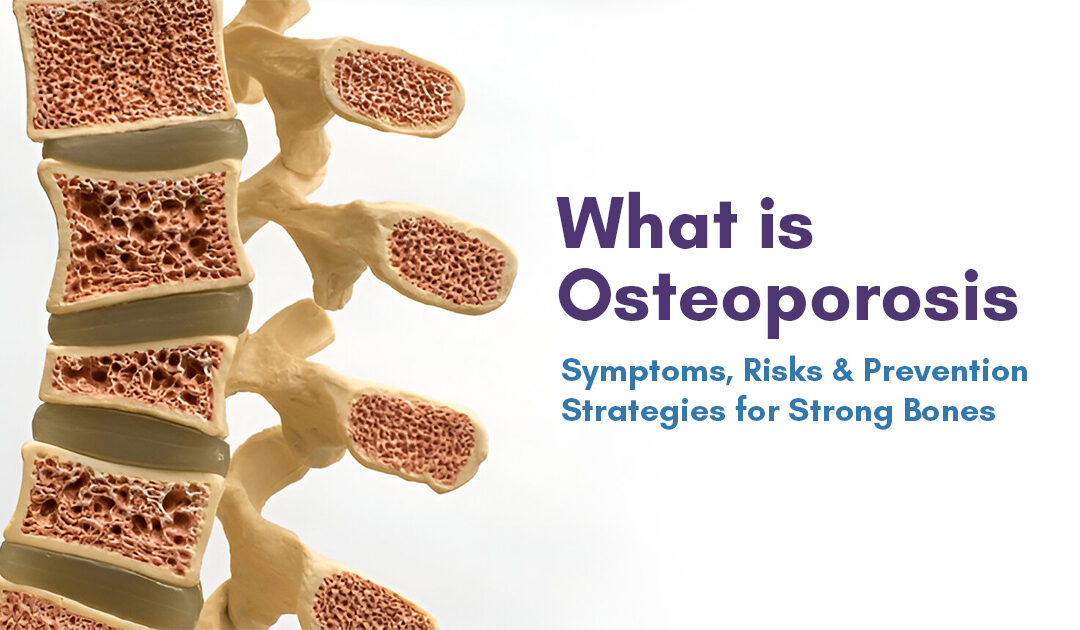
The bones in your body are living tissue that are constantly being broken down and replaced. When the creation of an old bone fails to keep up with the loss of an old one, that is when osteoporosis occurs.
Osteoporosis is the condition where bones turn weak and brittle to a point where even bending over could cause a breakage. This condition commonly occurs in the hip area, wrist, and spine. While osteoporosis doesn’t discriminate between any gender or age group, white and Asian women, especially those past menopause, are at its highest risk. One may prevent bone loss or strengthen pre-existing weak bones through various methods such as medicines, a healthy diet, and weight-bearing exercises.
Symptoms and Causes
Osteoporosis doesn’t have symptoms like other health conditions and is therefore called the silent disease. There are no signals or warning signs indicating osteoporosis. There is no fever, headache or stomach ache that can help you know if there is something wrong with your body.
In fact, the most common symptom is an unfortunate bone break, occurring after a minor fall such as slipping on something or a small accident.
However, it causes a few visible alterations in your body that you may notice despite not having direct symptoms. These changes may mean that your bones are losing strength or density. These signs may consist of:
- Losing an inch or more of your height.
- Changes in your natural posture (stooping or bending forward more).
- Dyspnea or shortness of breath (if disks in your spine are compressed enough to reduce your lung capacity).
- Lower back pain (pain in your lumbar spine).
It might be difficult to notice these changes in your own physical appearance; hence, check with your loved one if they see any changes in your body with your height or posture. If you experience any of these symptoms, consult with your healthcare provider for a bone density test.
As you grow older, your bones lose the ability to regrow and reform themselves. Since they are living like any other part of your body, they’re replacing their cells and tissues all through your life. Until the age of 30, your body has a natural tendency to build more bones than it loses. It is after the age of 35 that bone breakdown begins as your body fails to replace it, causing a gradual loss of bone mass. Women after menopause are more prone to losing bone mass faster.
Risk Factors:
There are many risk factors for osteoporosis. While it is true that anyone can develop osteoporosis, some are more prone to experiencing it, such as:
- People over the age of 50.
- People assigned female at birth (AFAB), especially those postmenopause.
- People with a family history (if someone in your biological family suffered from osteoporosis).
- People who are thin or with “smaller frames” have less natural bone mass, so any losses can affect them more.
- People who smoke or consume tobacco products.
Some health conditions can make you more prone to developing osteoporosis, such as:
- Endocrine disorders — any condition affecting your parathyroid glands, thyroid gland and hormones (like thyroid disease and diabetes).
- Gastrointestinal diseases (such as celiac disease and inflammatory bowel disease [IBD]).
- Autoimmune disorders affecting your bones (such as rheumatoid arthritis or ankylosing spondylitis—arthritis affecting your spine).
- Blood disorders (or cancers affecting your blood like multiple myeloma).
Some surgical procedures and medications can intensify your risk of osteoporosis.
- Diuretics (medications that lower your blood pressure and clear extra fluid from your body.
- Corticosteroids (medications that treat inflammation).
- Medications used to treat seizures.
- Bariatric (weight loss) surgery.
- Hormone therapy for cancer (including to treat breast cancer or prostate cancer).
- Anticoagulants.
- Proton pump inhibitors (like those that treat acid reflux, which can affect your calcium absorption).
Certain aspects of your diet and exercise routine can make you more likely to develop osteoporosis, including:
- Not consuming enough calcium or vitamin D.
- Leading a sedentary lifestyle
- Regularly consuming alcohol (more than two drinks per day).
Diagnosis and Tests:
Your healthcare provider may diagnose osteoporosis with a bone density test. This is an imaging test designed to measure the strength of your bones through X-rays, which show the levels of calcium and other minerals present in your bones. These scans are also called DEXA scans or bone density scans. It is an outpatient test, which means you could go home after you’re done.
Treatment:
You may treat osteoporosis by simply exercising regularly and taking vitamin and mineral supplements and medication for osteoporosis.
Prevention:
You may follow these safety steps to reduce the risk of an injury:
- Wearing a seat belt in car
- Wearing the right protective equipment in all sports and activities
- Decluttering your house so that you don’t trip over anything
- Consuming a proper diet
- Exercising regularly
Osteoporosis has no warning; it is important that you are aware of the changes in your body. If noticeable, contact a healthcare professional and tell them about any other symptom you’re experiencing, especially if it’s pain in the bones or you have mobility issues.